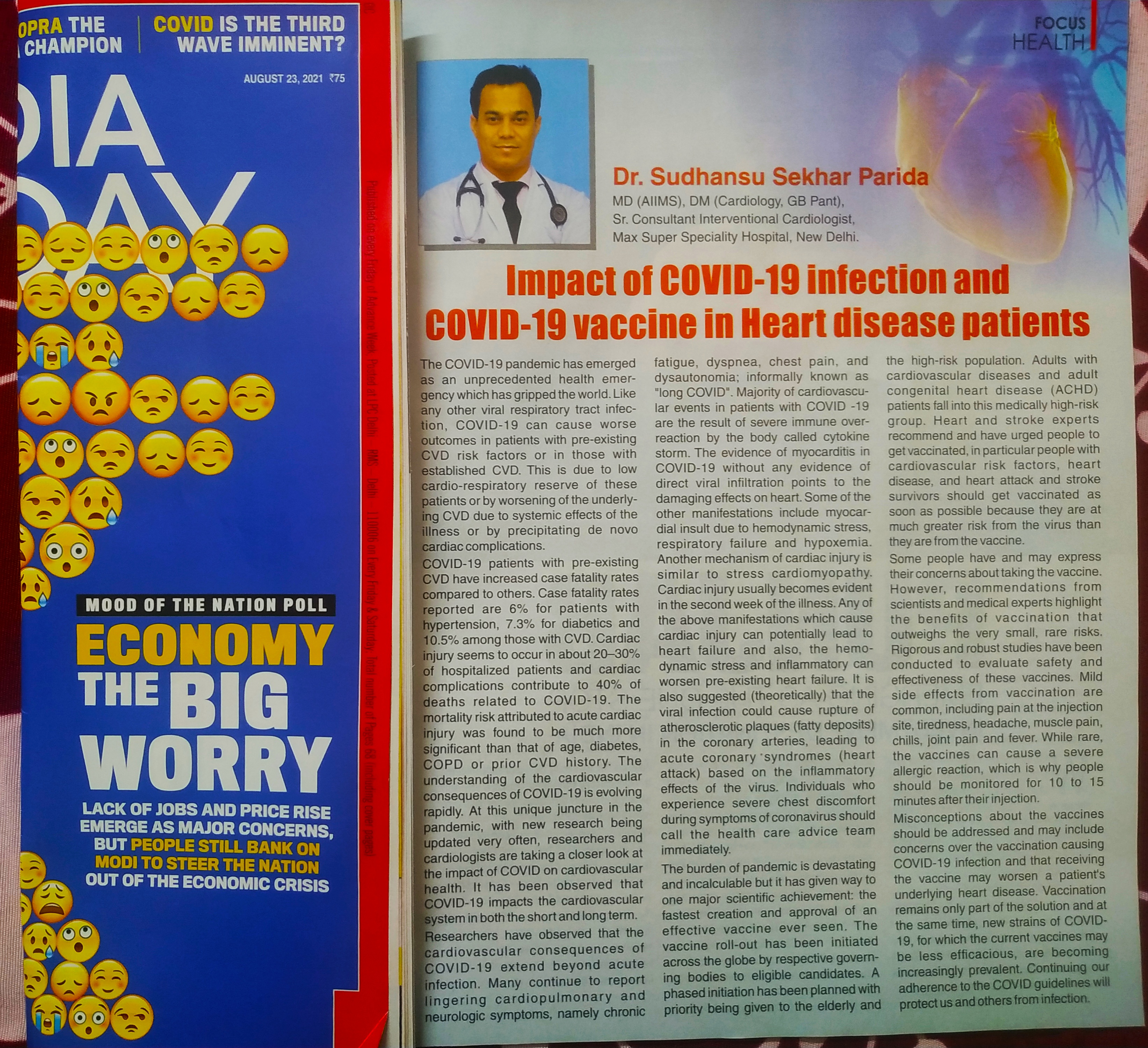
Dr.Sudhansu Sekhar Parida is one of the renowned Interventional Cardiologists in New Delhi. He is currently working as a Senior Consultant, (Interventional Cardiology) at MAX Super Speciality Hospital, Shalimar Bagh. He is highly qualified, having done his Post Graduation from most reputed institute of India - AIIMS Delhi and Super-speciality from G B Pant Hospital Delhi.
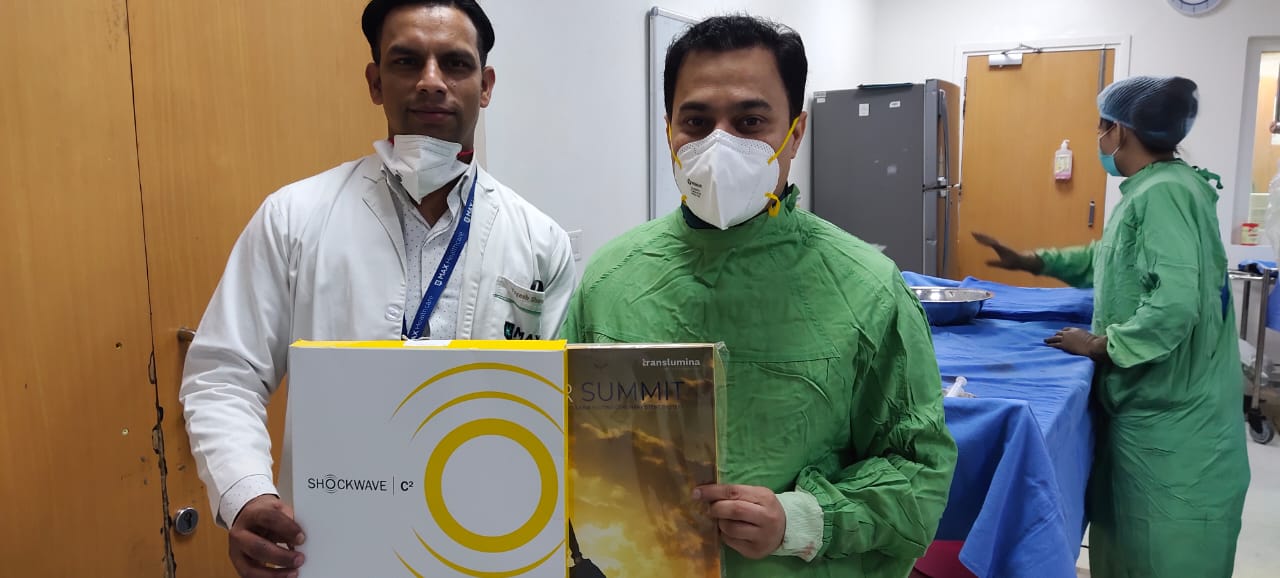
He has rich experience in Interventional Cardiology procedures and has performed more than 20000 angiographies & angioplasties as a primary operator. He is an expert in Transradial Angiography, i.e., angiography via the radial (wrist) route, which is considered to be safer and patient-friendly. He is well versed in all state-of-the-art technologies that include interventions like Rota Ablation, & Atherectomy, Fractional Flow Reserve (FFR), and intracoronary imaging like Intra Vascular Ultrasound (IVUS) and Optical Coherence Tomography (OCT). He also has experience in device closure for various types of congenital heart disease like atrial septal defects (ASD), ventricular septal defects, (VSD) & patent ductus arteriosus (PDA). He has also done numerous cases of ballooning of blocked valves like BMV, AVBD, PBVD. He also has immense experience and expertise with permanent pacemaker implantation, AICD, CRT-P, and CRT-D. Other interventions in which he has experience like peripheral, carotid, and renal angioplasties, IVC filter, PERMACATH insertion, etc.
We are committed to forming a true partnership with each patient as we strive to serve as guiding hands toward better health and a life lived to the fullest.